
If you have gum disease and are considering dental implants, you’re not alone — it’s one of the most common questions patients ask. The good news is that you can get dental implants if your gum disease is treated and stable. However, placing an implant while infection or inflammation is still active can lead to complications such as poor healing, bone loss, or implant failure. At Sohodent, we carefully assess gum health, provide targeted periodontal treatment first, and create a personalised plan to ensure your implants heal safely and last for years. This guide explains when implants are possible, how gum disease affects the process, and the essential steps to protect your new smile.



Having gum disease does not automatically disqualify you. What matters is whether your condition is active or stabilised. If your gums are inflamed, bleeding easily, or your pockets are deep, implant surgery should wait. Once periodontal therapy reduces inflammation and you can keep plaque under control, most patients become candidates. We assess oral hygiene, pocket depths, bone levels, smoking status, diabetes control, and medication history before recommending a plan.



When gum disease is treated and stable, implants are generally safe. Success depends on meticulous cleaning and follow-up. Our protocols emphasise pre-surgical debridement, atraumatic placement, and personalised aftercare. If you’ve had advanced periodontitis, we discuss additional maintenance to protect the implants long term.
Untreated disease can spread to the implant site, leading to peri-implant mucositis or peri-implantitis. Patients may experience swelling, bleeding on brushing, bad taste, or loosening over time. The good news is these risks drop sharply after stabilisation and with a strict home-care routine.


Active gum infection creates a hostile environment: more harmful bacteria, deeper pockets, and reduced immune control. Placing an implant in this setting increases early failure and late complications. Treating the gums first improves tissue quality, reduces bacterial load, and provides a stable foundation for osseointegration.
Typical pre-implant periodontal care includes:
Comprehensive cleaning and root surface debridement
Antibacterial mouthrinses or site-specific antimicrobials
Bite adjustments if trauma contributes to pocketing
Smoking cessation and diabetes optimisation
Re-evaluation to confirm inflammation control
If pockets remain after initial therapy, we may stage care — additional debridement, local antibiotics, or minor periodontal surgery — before planning the implant. This “treat-then-place” approach is key to safer outcomes.
Healthy gums support faster healing, less swelling, and easier hygiene access around the implant crown. Stabilised tissues also help you keep plaque away from the critical implant–gum junction, limiting long-term peri-implantitis risk.

Stabilising gum disease comes first. Once inflammation is controlled and hygiene is reliable, we confirm readiness before booking surgery. Use this quick checklist to see if you’re likely ready for dental implants with a history of gum disease.
| Factor | Target Before Surgery | Why It Matters |
|---|---|---|
| Bleeding on Probing | Minimal | Indicates controlled inflammation |
| Plaque Levels | Low and localised | Lowers bacterial load |
| Smoking | Stopped | Improves healing and blood supply |
| Diabetes Control | Stable | Reduces infection susceptibility |
| Home-Care Skill | Verified | Ensures daily biofilm removal |
If any items are off-target, we tailor additional periodontal treatment and re-evaluate—this staged approach improves implant success at Sohodent.
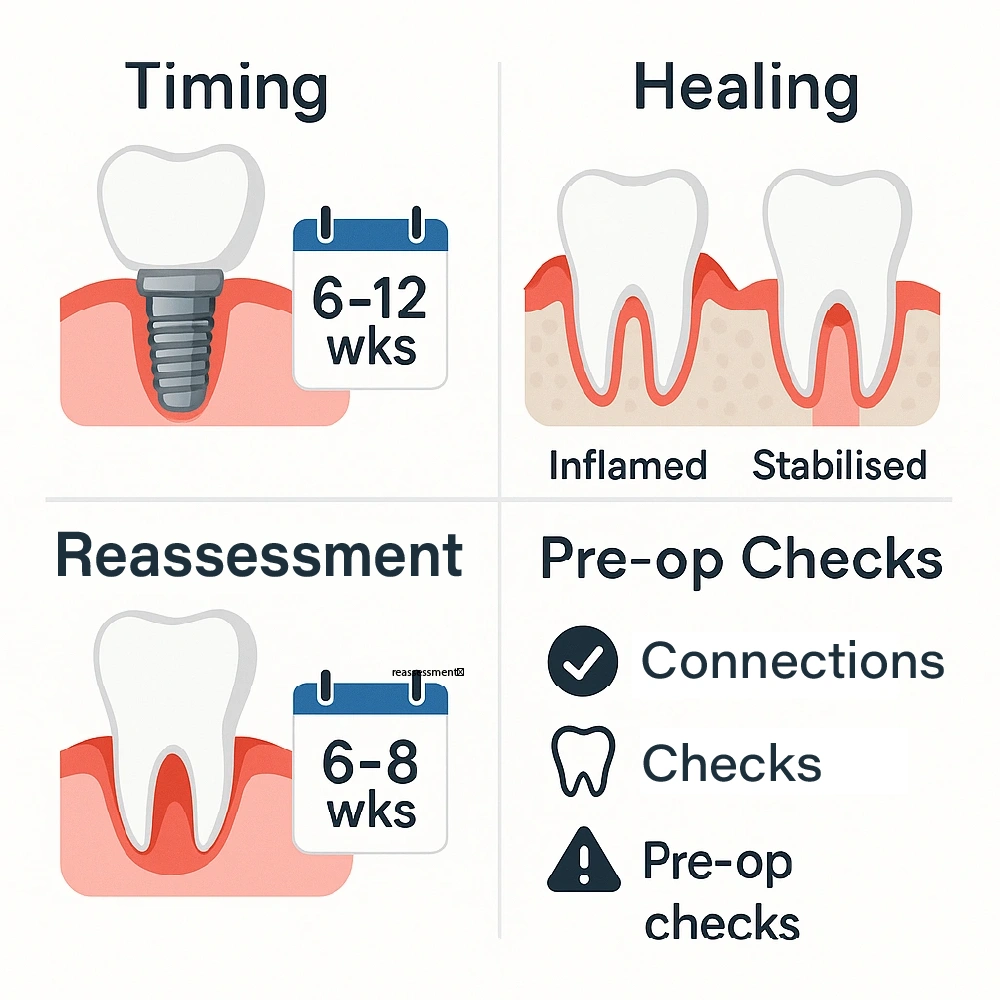
After non-surgical therapy, we typically re-assess at 6–8 weeks. If bleeding is minimal and pockets are shallow, we can plan surgery. After periodontal surgery or grafting, timing is personalised — often 8–16 weeks.
Inflamed tissues heal slower. Stabilised gums allow the body to focus on bone integration rather than fighting infection. That means a smoother recovery and fewer post-op issues.
Before booking surgery, we confirm:
Infection can occur early or late. Early issues often relate to surgical contamination or poor plaque control; late infections often follow lapses in cleaning or gum relapse.
Common triggers:
Late-phase risks include loosening screws from overload, residual cement trapping bacteria, and recurrence of periodontitis in neighbouring teeth that spreads to the implant.
Your personalised plan at Sohodent reduces these risks with antiseptic protocols, gentle suturing, clear hygiene coaching, and scheduled maintenance.

“An ounce of prevention is worth a pound of cure.” We combine aseptic surgery with patient coaching to keep the site stable.
Your immediate post-op checklist:
Diet progression for the first week:
In the first week, consistent home care and a gentle diet reduce infection risk and support osseointegration. Follow this simple timeline after your dental implant surgery.
| Day | What To Expect | What To Do |
|---|---|---|
| 1–2 | Mild swelling, oozing | Cold compress, soft foods, prescribed rinse |
| 3–5 | Discomfort decreasing | Gentle brushing near site, continue rinse |
| 6–7 | Bruising fades | Gradual return to normal diet, no hard seeds |
Questions or concerns during recovery? Contact Sohodent for personalised advice and a same-week check if needed.
At any stage of your journey, if you are unsure, Get in touch for your treatment plan. — our team can advise on safe cleaning and diet adjustments tailored to your case.
Prompt action keeps small problems small.
Contact us if you notice:
We may prescribe antiseptic rinses, targeted antibiotics, or perform professional cleaning around the site. The earlier we intervene, the simpler the solution.
If you suspect infection or trauma to the implant, call the clinic the same day. Out-of-hours guidance is available for urgent concerns in the UK, Ireland, and USA patient time zones.
Swift, structured care prevents escalation.
Antibiotics are sometimes appropriate, but they work best when combined with professional cleaning and strict hygiene. We select agents based on your medical history and the likely bacteria involved.
We use specialised tools and protocols to clean implant threads and the surrounding tissues without damaging the surface. In stubborn cases, minor flap access or decontamination methods may be recommended.
Your plan might include more frequent hygienist visits, custom brushes or floss aids, and bite adjustments if overload contributed to inflammation. If you need help choosing the right tools, reach out to us for your tailored dental care and we’ll tailor a kit for you.

Understanding complications helps you prevent them.
Potential issues range from mucositis (reversible inflammation) to peri-implantitis (bone loss). Early bleeding or tenderness is a signal to review your cleaning technique.
Relapse of periodontitis in your natural teeth can increase bacterial load around the implant. Consistent maintenance reduces this cross-contamination risk.
In advanced cases, bone loss may require regenerative procedures or component replacement. The best strategy is prevention plus early intervention.

Think of your implant as a tooth that needs lifelong care.
Key habits:
Your hygienist will monitor bleeding scores, pocket depths, and plaque levels, and coach you on technique improvements. Small tweaks make a big difference over time.
Lifestyle matters: quit smoking, manage blood sugar, wear a nightguard if you clench, and follow recall schedules. Consistent habits are the single biggest protector of implant longevity.

Some patients benefit from a phased or alternative approach to optimise success.
Uncontrolled diabetes, heavy smoking, immunosuppression, or a history of aggressive periodontitis may justify additional staging, longer healing, or alternative options while risks are reduced.
Where bone is thin or soft, we may graft first and place the implant after healing, rather than on the same day. This can increase predictability in periodontally compromised mouths.
Staged care can extend timelines and add cost, but it often saves money and discomfort by preventing complications. We provide transparent plans and timelines before you start.

Sohodent brings periodontal and implant expertise under one roof for coordinated, safer care.
From diagnosis to maintenance, your team works to a single plan — no gaps, no mixed messages, just integrated care focused on infection control and long-term stability.
You receive a written home-care plan, hygiene coaching, and timed reviews that match your risk profile. If you need help between appointments, we’re a message away.
Travelling or relocating? We can coordinate maintenance with partner hygienists and complete remote check-ins to keep your plan on track.

Can Implants Disease Or Fail If I Have Gum Problems?
If gum disease is active, yes — failure risks rise. Once treated and stable, many patients do well with careful maintenance.
What Are The Best Steps For Preventing Infection After Dental Implants?
Clean daily with the tools we recommend, attend maintenance visits, avoid smoking, and follow your diet and medication plan during healing.
Do I Need Antibiotics For Post Implant Infection?
Sometimes. They are one part of care alongside professional cleaning and improved home hygiene.
How Soon Can Implants Be Placed After Treating Gum Disease?
After non-surgical therapy, many patients are ready in 6–12 weeks; complex cases may need longer or staged grafting.
What Are The Post Implant Infection Risks If I Smoke?
Smoking increases infection and healing problems. Quitting before surgery and throughout healing is strongly advised.


Key takeaways: Treat the gums first, stabilise your oral health, and follow a strict hygiene and review plan. With this approach, most patients with prior gum disease can enjoy successful implants for years.
Next steps with Sohodent:
If you want a realistic timeline and costed plan, contact us to start your treatment. — we’ll guide you from stabilisation to restoration with evidence-led care.

